What is endometriosis?
Endometriosis is the growth of the endometrium (the tissue that lines the uterus) outside of the uterus. Most often, endometriosis is also found in other parts of the reproductive system, but in rare cases, it can happen throughout the body.
What causes endometriosis?
The endometrium in your uterus swells with blood and other tissues just before your period. If you get pregnant, this provides a good environment for a fetus to grow. If you do not get pregnant, the extra tissue is shed as menstrual blood.
When patches of endometrium grow in other parts of the body, however, they can cause the formation of scar tissue and make other organs stick together because the misplaced swollen endometrium is shed inside your body during your period just like the endometrium in your uterus. This can cause inflammation and pain.
Who is at risk for endometriosis?
About 5 million women in the United States are living with endometriosis. Some risk factors may put you at a higher chance of developing endometriosis, but endometriosis can happen to anyone who has menstrual periods, and it is most common in women aged 30-40. However, you may be more likely to develop endometriosis if you experience the following:
- Never had children
- Menstrual periods that last more than seven days
- Short menstrual cycles (27 days or fewer)
- A family member (mother, aunt, sister) with endometriosis
- A health problem that blocks the normal flow of menstrual blood from your body during your period
Research also shows a link to other health conditions in people living with endometriosis, like asthma, chronic fatigue syndrome, fibromyalgia, autoimmune diseases, and some cancers. While you can’t exactly prevent endometriosis, you can try to reduce your chances of developing it by lowering your estrogen levels, a hormone that helps thicken the lining of your uterus. This can be achieved by using a specific type of birth control, exercising, and avoiding excessive amounts of alcohol and caffeine.
How does endometriosis affect fertility?
Many people living with endometriosis are able to become pregnant, but it’s possible you may find it harder. Research shows that half of women with infertility also have endometriosis. Fertility can depend on factors like your age, your partner’s fertility, and how severe the endometriosis is. While experts don’t exactly know how endometriosis affects fertility, it’s possible that endometriosis may change the shape of the pelvis and reproductive organs, or be related to the immune system and endometrium. It may also be related to fallopian tube scarring, hormonal changes to the environment of the eggs, or altered egg quality. Because tissue that should be growing on the inside of the uterus is growing on the outside, the growth may block your fallopian tubes or cover your ovaries.
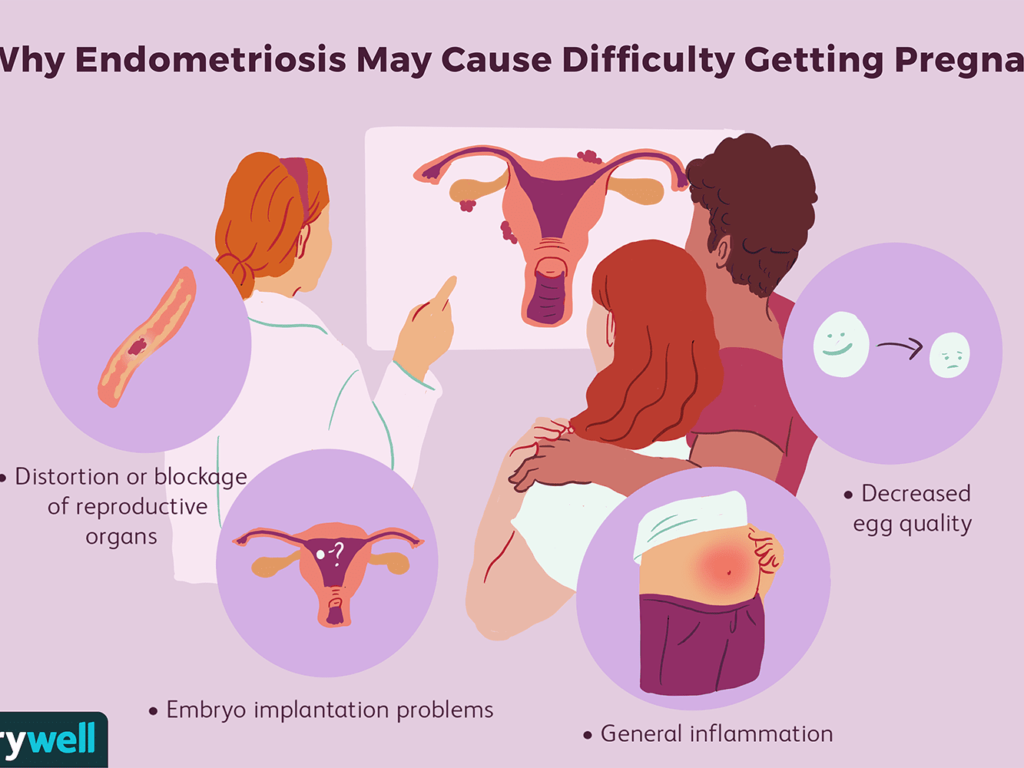
(image from VeryWell, Colleen Tighe)
If you’re wondering if you should attempt to conceive naturally while living with endometriosis, experts say yes! Endometriosis does not automatically mean you can’t become pregnant, and if you’re experiencing difficulty conceiving, speak with your doctor as there may be treatment options available to help you. Generally, people with endometriosis are advised to try conceiving for six months before exploring fertility treatment, but some decide to pursue other options right away. Additionally, since fertility declines after age 35, some people in their 30’s may not want to wait. Click here for a Doctor Discussion Guide for help talking with your doctor about fertility and endometriosis.
Endometriosis and abortion
Having an abortion does not cause endometriosis. This myth has been perpetuated by opponents of abortion who lashed out on social media following a Democratic National Convention speaker who in 2012 shared her experience accessing care for endometriosis at Planned Parenthood. In fact, it’s been proven that women with endometriosis have had fewer pregnancies, elective abortions, or ectopic pregnancies compared to those experiencing infertility without having endometriosis. While endometritis, an illness characterized by the inflammation of the lining in the uterus, can be associated with procedures like a surgical abortion, the worldwide rate of infection following an abortion is rare. The idea that a person did something to cause their endometriosis is incorrect because although endometriosis does run in families, doctors aren’t sure what causes it. And while endometriosis has been associated with surgical scar implantation, like endometrial cells attaching to a surgical incision, it’s important to remember a surgical abortion is not actually surgery. No incisions or cutting takes place during the procedure.
What are endometriosis symptoms?
You may consider getting an endometriosis test if you have any or all of the following symptoms:
- pain in the abdominal area and lower back, mainly during your period, but much worse than typical menstrual cramps
- pain from sex
- diarrhea, constipation, or nausea
- fatigue
- infertility or difficulty conceiving
Endometriosis may also be linked to other chronic health problems such as autoimmune diseases, chronic fatigue syndrome, fibromyalgia, allergies, and certain cancers.
Should I get an endometriosis test?
If you have any of the above symptoms, talk with your doctor or your obstetrician/gynecologist (OB/GYN) who has special training to identify endometriosis, which can be mistaken for other problems.
During your endometriosis test, an OB/GYN uses tools such as ultrasound and pelvic exam to look for more symptoms associated with endometriosis, but the doctor must look inside your abdomen to know for sure. Fortunately, there is a relatively easy way to do that, called laparoscopy, in which the doctor makes a small cut in your abdomen and inserts a small tube with a camera and a light to look inside for growths.
What treatment is available for endometriosis?
Unfortunately, there is not a known cure for endometriosis, but some growths can be removed surgically with laparoscopy, and there are other treatments that can help reduce pain and reverse infertility, such as hormone therapy. You should discuss your options with your doctor.
Endometriosis resources
- American Congress of Obstetricians and Gynecologists: Pamphlet on endometriosis
- The National Women’s Health Information Center: Frequently Asked Questions about endometriosis